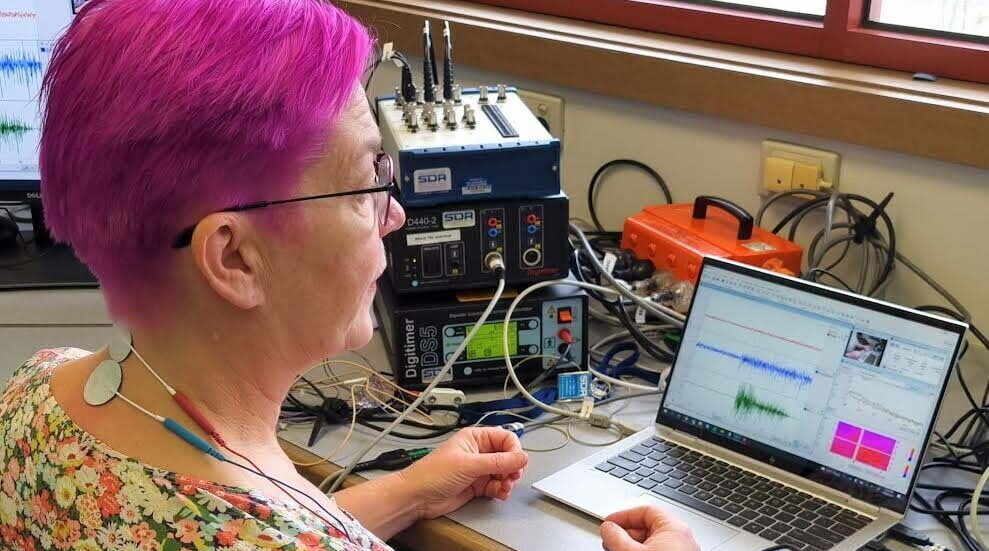
Researcher Mary Galea
Story by Grant Maynard
When it comes to nerve pain and function, ideas and concepts can become complex quickly. In its simplest form, an off-the-shelf $60 TENs unit is a form of stimulation via electrodes. Aiming to reduce nerve pain by placing electrodes across the skin to stimulate the nerves which then, hopefully, increases and improves function.
While extremely crude in its approach, especially when compared to other options, a basic TENs unit can make a huge difference for nerve pain and pain management, for others its just a $60 paper weight.
The next step can then feel like a monumental jump to an implanted device (Spinal Cord Stimulator) with cables running through the affected areas to stimulate the nerves. While these devices get better each iteration with wifi controls, longer batteries, test periods and more, it comes with a significant cost well over $5000, so what if there was another way?
A new study looks to replicate these results of an implanted device using external methods only, to achieve a similar result and improve (specifically) upper limb function, ie. your arms and hands.
Professor Mary Galea from the University of Melbourne is leading a study to test a new option to achieve this for people with a spinal cord injury.
Let’s get some tech-speak out of the way first, what is Neuromodulation?
Neuromodulation is the alteration of nerve activity through targeted delivery of a stimulus, such as electrical stimulation to specific parts of the nervous system.
How is your proposal and study different?
Transcutaneous electrical spinal cord neuromodulation (TESCoN) is a non-invasive form (not requiring surgery) of neuromodulation in which electrodes are placed on the skin over the spinal column and used to stimulate the spinal cord via an electrical current (ie: a system that affects the nerves under the skin). This electrical current targets spinal cord pathways that have been spared from the injury, but are not working normally, though this type of stimulation does not target motor responses directly.
If this approach doesn’t target motor responses, how do you hope to improve upper limb function?
This approach activates networks within the spinal cord, such as central pattern generators and the propriospinal system. A central pattern generator is a network of neurons capable of generating a coordinated rhythmic motor pattern, such as walking or breathing, in the absence of input from the brain and/or peripheral stimuli from the skin, muscles or joints.
The propriospinal system comprises of neurons and link circuits that control the movements of the limbs and the trunk.
Modulation of these spinal networks by TESCoN raises the baseline excitability level so that the spinal circuitry below the injury requires smaller levels of excitation to start working.

So, in a way you’re hoping to stimulate and excite one nerve group, to elicit a response and movement from another?
After a spinal cord injury, the excitability of the networks within the spinal cord is low, so it is difficult to activate undamaged pathways. Stimulating the spinal networks can raise the general level of excitability within the spinal cord. Movements can then be generated by the individual with spinal cord injury because the level of excitability is raised above the threshold required to elicit movement.
Intensive rehabilitation combined with TESCoN enables a change in the connections within and between the networks involved in controlling movements (called activity-dependent plasticity), resulting in improved function. TESCoN on its own is insufficient to lead to functional recovery. It enhances the effect of intensive rehabilitation and is not a replacement for it.
You mentioned function, at the end of the day that is what people are really looking at. What functional changes should people expect from this approach?
Recent studies in people with chronic tetraplegia have shown that TESCoN plus intensive rehabilitation can promote lasting recovery of upper limb function to a greater degree than rehabilitation alone.
What do you hope to achieve from this study?
This trial is a Phase 2 trial, i.e. an early phase trial designed to investigate the safety and preliminary efficacy of TESCoN. This will enable us to examine whether similar outcomes occur in those who are recently injured compared to those who have had their injury some time ago. A successful outcome of this study will provide the basis for a future multi-site trial in the Australian and international spinal cord injury community.
After the research is completed, when are people likely to be able to find out more?
The trial is expected to take 5 years to complete, at which time the results will be made publicly available.
How to get involved
To be eligible:
- You have tetraplegia below C4 as a result of traumatic spinal cord injury
- The time since your injury is 3-6 months, or 12 months or more
- You are aged between 15 and 75 years
- You do not have any other neurological condition or injury
- You do not have any implanted device (e.g. pacemaker)
What would happen if I took part in the research study?
If you decide to take part in the research study, you will be asked to attend the Royal Talbot Rehabilitation Centre for screening, medical clearance and other assessments, then attend Monday to Friday for a period of 4 weeks to receive TESCoN plus intensive therapy for your arm and hand. You will be re-assessed after the intervention, and again at 3 months. Each session will take 2-4 hours.
Will I be paid to take part in the research study?
You will be reimbursed for any reasonable travel, parking and refreshment expenses.
Who do I contact if I want more information or want to take part in the study?
If you would like more information or are interested in being part of the study, please contact:
Dr Maya Panisset
Department of Medicine (Royal Melbourne Hospital)
[email protected]
0405 027 127
- August 18, 2022